Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Overview of treatments for Benign Prostatic Hyperplasia (BPH)

Consultant Urological Surgeon
Kings College Hospital NHS Trust retired but still working privately
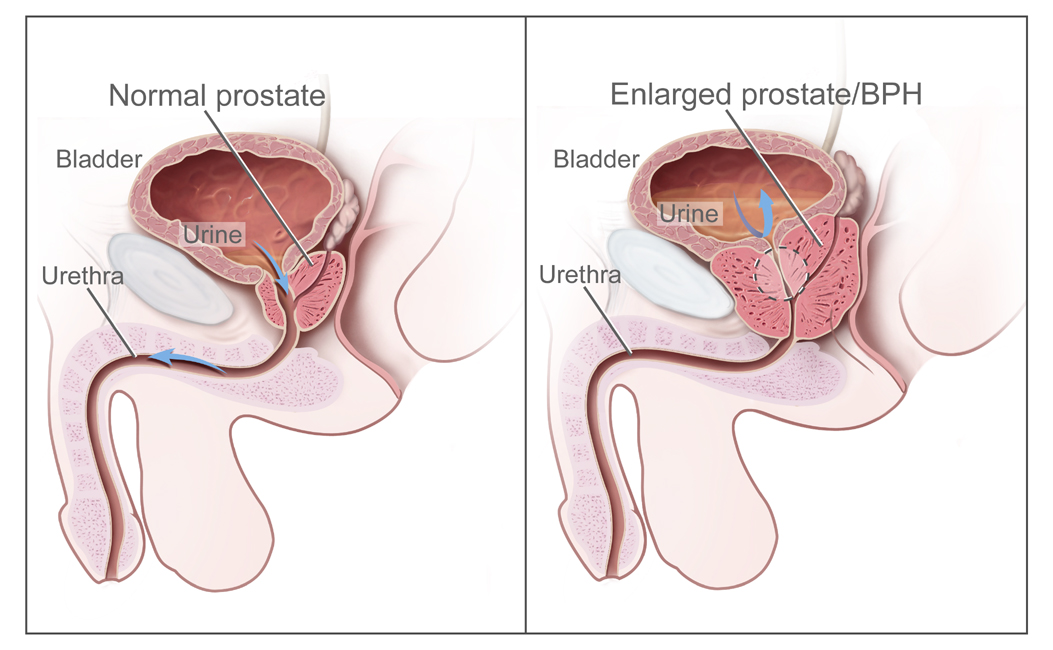
Overview of treatments for Benign Prostatic Hyperplasia (BPH)
Until only a few years ago, most men with prostate problems would have been offered the choice of
medication or one type of operation. While surgery in the form of TURP is a very effective treatment which
has stood the test of time, it is an operation which does require a few days in hospital and which does have
a risk of significant bleeding and where a significant majority of men will develop a permanent dry orgasm
and a small number of men will develop erectile dysfunction (with an even smaller chance of surgical
incontinence. ) Over the last 5-10 years the landscape has changed almost beyond recognition in terms of
the choices available to men although sadly a study my group published last year showed that most
urologists do not even consider sexual side effects of their patients when offering treatment for benign
prostatic obstruction. (World Journal of Urology [21 Apr 2018, 36(9):1449-1453)
I wished, in this article, to outline the ways in which men may be best selected for the different operations
and treatments we now have, and to explain why some procedures may be more suitable for some men
than others.
Treatments for benign prostatic obstruction can now be divided broadly into four groups. Some treatments
make incisions or cuts into the prostate and bladder neck, some treatments hold the prostate or bladder
neck open, others shrink the prostate without immediate tissue removal and the last group creates an
immediate cavity in the prostate. As you will see later on, these techniques are further sub-divided.
In our practice, when a man comes along who has made a decision that medical therapy isn’t enough for
him (or men who have retention with failed removal of a catheter), we will usually be asking about his
general health status and desire to maintain sexual function before looking at the man’s prostate itself.
Some men are surprised by this approach but in general, we can get almost all man passing urine
comfortably without a catheter nowadays and any residual bladder symptoms following prostate treatment
can usually be fixed. There is of course the occasional patient for whom we cannot get a perfect outcome.
Some of the treatments available have lots of high-quality randomised evidence supporting them and some
do not. In my summary of each of the treatments given below, I have tried to give an objective view but
this is not an exhaustive scientific appraisal of each treatment, so please do not take me to task! Very few
treatments have evidence across all patient groups and all complications.
Techniques that make or cuts or incisions into the prostate or bladder neck
The classic procedure here is the bladder neck incision or prostatotomy which has traditionally been carried
out by either one or two cuts in the prostate using an electric knife under general anaesthetic. Classic
bladder neck incision usually involves 1-2 nights in hospital, has a low risk of bleeding and has been shown
to be roughly equivalent to TURP surgery in the first few years. For smaller prostates. It is generally used
only in smaller prostates without significant middle lobes. Men who have the procedure have a very small
chance of developing surgical incontinence and there should be no significant risk of erectile dysfunction
unless the operation is done very aggressively. Many surgeons will now use laser (holmium or GreenLight
laser are both used commonly) for bladder neck incision which usually means the patient can go home the
same day, often without a catheter. The major downside of bladder neck incision is about a 15% chance in
most series reported of permanent dry orgasm and if this occurs, it is not reversible.
iTIND:
The iTIND is a new device which looks a little like the cage on a champagne cork and which is placed into
the prostate under local anaesthetic. Essentially it has three small spring bars on it which applies gentle
pressure onto the inside of the prostate over a week – it is then removed under local anaesthetic. The end
result is that three small incisions (a bit like a Mercedes Benz badge when seen through the telescope) are
made in the prostate and this allows symptom relief in the first year, not dissimilar to that seen with bladder
neck incision or TURP. No cases of sexual function or dry orgasm have been reported with the iTIND so
far although its use has been limited to relatively small prostates and data with larger prostates is not
available. Trials are currently running in looking at the iTIND in men with retention of urine. The long-term
revision rate of the iTIND isn’t known as it is new but the short-term re-operation rate would seem to be in
the order of 3-5% per annum going forward.
Neither bladder neck incision nor iTIND affects future revision surgery.
Stents and suturing techniques
There are a number of techniques that have tried to hold the prostate open without removing tissue and
these have had varying degrees of success over the years.
UroLift:
The UroLift procedure has gained attraction over the last 5-6 years and is essentially a device which allows
quilting stitches to be placed in the front of the prostate, giving an anterior prostate channel (the anterior
urethral lift) and is a simple procedure, carried out usually under light anaesthesia or IV sedation although
some centres have had success with local anaesthetic. My personal experience with local anaesthesia
means I generally advise a light sedation as well as local anaesthesia. Essentially the UroLift places
between 2 and 6 (occasionally more) small stitches holding the channel of the prostate open and fairly
instant relief is given for most men. Comparative trials have been carried out between UroLift and TURP
and have shown good patient outcomes in most groups with the UroLift not giving quite the same degree of
symptom relief or disobstruction but with very little time in recovery and with no reported cases of
ejaculatory or erectile dysfunction (indeed there was a marginal improvement in sexual dysfunction for men
having had UroLift). The re-treatment rate with UroLift runs at about 20% at 5 years and it is probably
somewhat less suitable for very large prostates. A large middle lobe of the prostate is a relative
contraindication to UroLift although some UroLift doctors have tried to develop techniques to try to stitch the
middle lobe and avoid this problem.
For all those patients to whom the UroLift isn’t effective or the symptoms recur, the presence of UroLift
does not interfere with any other potential operations. Because UroLift does leave small metal implants in
the prostate, it may not be suitable for those men who wish to go onto monitoring of prostate cancer or
potential prostate cancer, and this needs to be discussed with physicians who are expert in treatment of
localised prostate cancer.
Intraprostatic stents:
A number of stents (premanent or temporary devices to hold open the channel of the prostate) have been
tried over the years, typically in very unfit patients. Now that even laser prostatectomy can be carried out
in men with severe comorbidities in great safety, the rationale for using minimal procedures for unfit
patients is probably less important. Metal stents have been used which lie inside the prostate as a
permanent spring (Memokath) and have also been trialled as permanent stents which become enmeshed
within the prostate (UroLume or Memotherm). Few surgeons are now using stents due to problems with
migration and also in those stents where the stent was permanent, there have been many major problems
with overgrowth of the stent which can be very difficult to remove. Nonetheless, there may be an option,
depending on the environment for men in retention of urine who were not felt fit for general anaesthesia.
Occasionally they were used in the past for men wishing to try to preserve fertility but newer techniques
have very much superseded that indication.
Cavity Forming Techniques
There are a number of techniques to form instant cavities within the prostate. This can be carried out by
electrosurgery, laser therapy or most recently, high pressure water jets. A brief guide as to these
techniques is given below. Every one of them gives early and dramatic relief of prostatic obstruction but
varying amounts of tissue are removed from each and the side effects and hospitalisation vary slightly
among them.
For men in acute retention of urine, TURP and laser prostatectomy will have a better than 90% chance of
getting rid of the catheter.
REZUM (interstitial water vapour therapy)
Here, steam is injected into the prostate- this can in some units be done under local anaesthetic as an
outpatient
A catheter is needed for some days and it can take a few weeks to see results, but the end process is a
small cavity in the prostate with tiny risks of incontinence or erectile problems and about a four per cent risk
of a dry orgasm.
Trans-Urethral Resection of the Prostate (TURP):
This has been the standard of care now for many decades in Western countries and involves a telescope
being inserted through the eye of the penis and use a superheated electric wire which allows small pieces
of prostate (these look a little like pieces of mince) to be removed step by step from the prostate. TURP
used to be carried out using a technique called monopolar diathermy which had a risk of a complication
known as TUR syndrome- is now usually carried out using a bipolar diathermy system which avoids that
choice. In most centres, TURP still requires 2-3 days in hospital since often the bladder needs to be
washed out for a while using saline following the operation. There is a modest risk of bleeding requiring
either bladder washout for clots or blood transfusion although with modern techniques, this risk is low. The
majority of men who have classical TURP will develop a dry orgasm and a small percentage of men
develop erectile dysfunction. In skilled hands, the rate of incontinence is low, no more than 1%. TURP is
usually not used for prostates greater than about 80g in size (this is 4-5 times the size of a normal 20g
prostate) due to the risk of absorption fluid and excess bleeding but some experts with bipolar systems will
go higher than this.
Electrovaporisation of the Prostate
Vaporisation of the prostate can also be carried out using electrosurgical systems, almost always bipolar
and results are similar to classical TURP although there has tended to be a slightly reduced amount of
tissue removed compared to the standard operation- whilst bleeding appears a little less, some studies
have shown a slightly higher risk of pain following the operation.
Laser prostatectomy can be carried out using two different techniques; the first is vaporisation where a
laser is used to turn tissue into steam creating a cavity and the second, by enucleation where the laser is
used as a knife to remove large chunks of the prostate which are then removed from the bladder using
tissue destruction device inserted through the telescope called a morcellator. A number of high-powered
lasers exist; the best studied being the holmium laser, the GreenLight laser and the thulium laser. Each of
these lasers can be used depending on settings for either the operations and can also be used for a
technique called vapor-resection which uses the laser to cut small chunks out, similar to a TURP, but is not
enormously popular in the majority of developed countries.
Laser vaporisation of the prostate:
this is most commonly carried out using the GreenLight laser although it can be done with other lasers.
Essentially, the laser is used to take away layers of the prostate through the telescope and in most
published series (there is randomised evidence comparing GreenLight laser vaporisation to TURP) it takes
away about 50% of the prostate and has an extremely low chance of bleeding with well under 1% of
patients requiring intervention. The majority of patients can go home on the same day or with a short
overnight stay and it is possible with laser vaporisation (this has also been reported by a few centres with
TURP) to try to reduce the risk of dry orgasm. We quote men a dry orgasm risk of about 13%, if ejaculation
preserving procedure is offered to the patient. A large number of men can go home the same day without a
catheter but some do need a small catheter for a few days. One of the benefits of the procedures that
could be carried out with relative safety in anticoagulated patients and (like all other lasers), can be safely
used in men with pacemakers or implantable electronic devices such as defibrillators. The success rate of
laser vaporisation in men with retention of urine is very high, certainly above 95% in most series and the
reoperation rate depends to a degree on how much tissue is removed but in our international group’s
figures, around 1`% of men per annum will need a revision operation after this surgery.
Prostate enucleation (usually HoLEP)
Anatomical endoscopically enucleation of the prostate (AEEP) is usually carried out with laser although
certain groups have shown it can be safely done by bipolar electrical treatment. All 3 of the main lasers
can be used for AEEP but the HoLEP procedure is by far the most widely studied and adopted enucleation
procedure and has been shown in randomised trials to be at least equivalent to the TURP operation in
terms of bleeding and recovery with more tissue removal. HoLEP has also been shown to be equivalent to
open prostatectomy (a technique mentioned only in my view for historical reasons or rank of technology).
The success of HoLEP in men with retention with a urinary catheter is close to 100% of men and the
reoperation rate is the lowest of all techniques available.
A number of men will have a degree of stress incontinence after full prostate enucleation but this tends to
improve although perhaps 1-2% of men will have some ongoing stress incontinence after enucleation of
large prostates and of course this can be treated. The risk of erectile dysfunction is low but with full
enucleation, the risk of dry orgasm is high and some groups are working to try to develop a solution to this.
Aquablation
This operation uses a robotically controlled high pressure water jet inserted and controlled by
predetermined ultrasound images. It is a very new development and seems in the short term to equivalent
to TURP with a lower risk of dry orgasm. One of the better advantages of the aquablation technique may be
the limited skillset needed: this may help in reproducing results (a problem that has dogged other new
techniques since varying levels of surgical skills are required for a good outcome). Aquablation is carried
out under a full general anaesthetic with usually a one night stay as patients require electrosurgical
treatment for bleeding at the end of the procedure.
While acquablation has no long term follow up, it seems that a larger volume of prostate is removed than
with most other techniques yet the dry orgasm rate is below 10%. Long term data on re-operation will take
a while to see. Incontinence and erectile dysfunction seem very rare.
Summary
We have a number of excellent treatments for men with benign prostatic outflow obstruction and nearly all
men now can be helped enormously by one technique or another. There is no right or wrong technique for
every single man and whilst some of the techniques mentioned above will not be suitable for everyone, it
will be unusual for there not to be several choices given to men who are concerned about the effects of
treatment on their quality of life.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

