Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Treatment of BPH – Aquablation therapy

Consultant Urological Surgeon
Norfolk and Norwich University Hospital NHS Foundation Trust
Aquablation treatment for enlarged Prostate
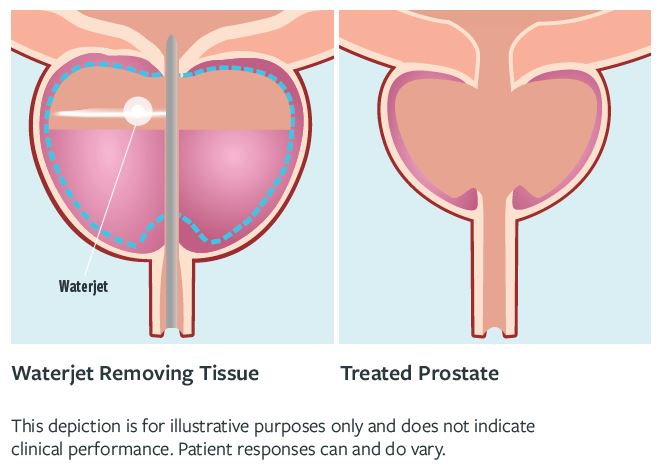
Aquablation treatment for enlarged Prostate or Aquablation therapy of the prostate using the ‘AquaBeam’ Robotic system, is a another novel alternative to TURP for BPH. It was developed by PROCEPT BioRobotics and uses real-time ultrasound scan images in combination with direct visualization to plan and deliver the treatment required. The system uses a high-velocity sterile heat-free waterjet and autonomous robotics, pre-programmed by the Urologist, to remove prostate tissue and create a TURP – like defect through the prostate. I mention TURP as clinical trials have used that procedure as a comparator.
The pre-programming defines the angle of the probe and the depth and duration for firing the water jet. As mentioned, a clinical trial comparing this to TURP in 30-80ml prostates showed that it can achieve symptom and flow improvement to at least as good a level as TURP (the reference standard), with similar re-treatment rate at 5 years. Surgical retreatment was 5% for aquablation at 5 years and 1.5% for TURP, although medical treatment more common in the TURP arm, accounting for the similar reported retreatment rates. (Gilling CJU 2022 ). A further single-arm study of larger prostates up to around 150ml (average size 107ml) showed similar effects, with a 3% surgical retreatment at 5 years and further 6% on medication (Bhojani J Urol 2023). An ongoing study is comparing its effect to that of HOLEP, but is not yet reported.
The procedure is usually performed with the patient under general or spinal anaesthesia. Whilst the ablation time is usually less than 10 minutes, the set up and real time ultrasound guided planning mean that the whole procedure takes about 45 minutes. At the end of the procedure, focal “bladder neck cautery” with a diathermy loop similar to that used for TURP is now recommended to stop bleeding. Once the procedure is complete a 3-way Foley catheter is placed through the penis into the urethra to ‘irrigate’ the bladder. The catheter is usually removed the next day and the patient is typically discharged from hospital once urine has been passed in an adequate fashion, although for some patients, the procedure is now done as a daycase, with the catheter removed at home or in a clinic after 24-48 hours.
The advantages of Aquablation therapy
- The consistency of treatment delivery
- the speed of the procedure almost whatever the size of the prostate
- It is largely heat free, other than the focal cautery phase, perhaps reducing the risk of complications from thermal injury and damage.
The procedure is very unlikely to result is erectile problems (<1%) and has a low incidence of dry ejaculation at 8%-15% depending on the study
The disadvantages of Aquablation
- There is a higher risk of bleeding than with other techniques, although the introduction of cautery to the procedure has reduced the transfusion rate from 3.9% to 0.8% (Elterman CJU 2021)
- In a similar manner to TURP, it does not remove the entire obstructing “transition zone” of the prostate. While some preservation of tissue may account for the lower rate of dry ejaculation, the trade off in the longer term may be a higher re-treatment when compared, for example with enucleation techniques such as HoLEP. Ongoing studies should address this.
- The procedure always requires catheterization with bladder irrigation and often an overnight stay in hospital, although some surgeons are now delivering this as a daycase procedure
HoLEP Vs Aquablation
Holmium laser enucleation (HoLEP), which is the standard option for men with larger prostates, can be performed as a day case with a very low rate of bleeding requiring transfusion.
A study published May 24 compared the outcomes of Aquablation and holmium laser enucleation of the prostate (“HoLEP”) in a prospective cohort.
Patients with BPH underwent Aquablation or HoLEP according to their preference between June 2020 and April 2022. Prostate volume (“PV”), laboratory results, postvoid (after urinating) residual urine volume, uroflowmetry (rate of urine flow), IPSS, (the International Prostate Sympom Score) ICIQ-SF, (The International Consultation on Incontinence Questionnaire), MSHQ-EjD (Male Sexual Health Questionnaire – ejaculatory dysfunction (EjD) Short Form), EES (extravascular-extracellular space) and IIEF (International Index of Sexual Function) were evaluated preoperatively and at three, six and 12 months postoperatively. Perioperative characteristics and complications were also analysed via the Clavien Dindo („CD“) classification of Complications Developed following Laparoscopic Urological Operations such as HoLEP, Greenlight laser, Aquablation etc.
40 patients** were included, 16 of whom underwent aquablation and 24 HoLEP. Mean age was 67 years. Baseline characteristics were balanced across groups, except the HoLEP patients’ larger prostate volume. IPSS score fell from 20.3 at baseline to 6.3 at 12 months without differences between aquablation and HoLEP. HoLEP was associated with shorter operation time (59.5 minutes vs. 87.2 minutes and led to better prostate volume reduction over all timepoints. At three months, Aquablation’s results were better regarding ejaculatory and continence function. However, beyond three months, erectile, ejaculatory, continence function and LUTS reduction did not differ significantly between Aquablation and HoLEP. Significant complications (Grade 3b*) were noted in six patients in Aquablation group while only one in HoLEP group.
*Grade 3 complications include situations where medical treatment is inadequate and requires surgical or endoscopic intervention. There are 2 subclasses of Grade 3. Grade 3A complications are intervened under local anesthesia and Grade 3B includes conditions intervened under general anesthesia.
**Note this is a small sample size. Results from larger studies which may indicate different results are expected in the future
Conclusions from this study
While Aquablation revealed temporary benefits regarding ejaculation and continence at three months, HoLEP was superior concerning operation time, the safety profile and volumetric results.
However, there was a meta study which included patients up until August 23 which had different results. Is this due to smaller average prostate size in the meta study? Also, it was not a direct comparison.
Meta study conclusions
Aquablation results in lower improvement in voiding parameters than HoLEP. It also has less sexual function decline than HoLEP, although not significant. Aquablation is associated with shorter operative times, longer postoperative catheterization and hospital stays and favorable serious adverse events rate compared to HoLEP. HoLEP has lower surgical RT than aquablation.
References

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media


