Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Advances in Transperineal biopsy techniques

Professor Frank Chinegwundoh MBE
Consultant Urological Surgeon
St Bartholomew’s Hospital
Barts NHS Trust
Due to the limitations of transrectal prostate biopsy (lack of access to the anterior prostate, infection risk), most urological surgeons now use transperineal prostate biopsy. Because the needle does not go through the rectum, the risk of sepsis is lessened.
The traditional technique of transperineal biopsies of the prostate involves sampling the prostate using a template attached to an ultrasound probe with holes every 5mm. This is known as a saturation, or template guided transperineal biopsy. This involves taking many cores, anywhere between 20 and 50. It is generally performed under general anaesthesia or spinal anaesthesia.
Saturation transperineal biopsy is being superseded in many centres by transperineal biopsy under local anaesthesia. The whole prostate gland can be sampled or abnormal areas seen on a mpMRI scan targeted cognitively. This has been facilitated by the advent of the ‘precision point’ device, which is placed on the transrectal ultrasound probe and acts as a needle guide.
With advances in mpMRI, very experienced physicians use ‘cognitive fusion’, that is, superimposing the MRI scans onto the ultrasound images “from memory” and in real time. The suspect areas detected during the MRI do not appear on the ultrasound images. In the hands of very experienced practitioners, this technique is very good and requires far fewer cores to be taken, as it is the suspicious areas on the mpMR scan that are sampled
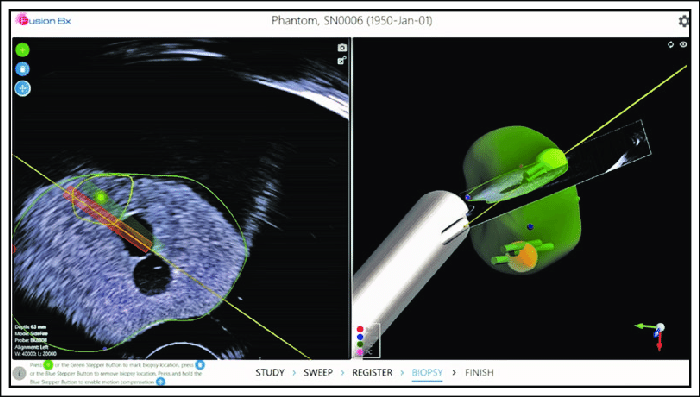
Cognitive fusion is increasingly being replaced by fusion software systems. This involves mapping the MRI image showing the location of potential cancer lesions, onto the the realtime,’live ’ultrasound image being produced by the probe inserted inside the rectum (endorectal).
The development of these systems has not been without its problems. Firstly, an MRI image is taken in a different plane to the live realtime ultrasound image, therefore complicating the process of superimposing one image on top of the over. This is essential in order to guarantee that samples are taken from the potential cancer sites.
There are also further issues that need to be taken into account to ensure accurate overlay.
- The prostate is a flexible and mobile organ and during a biopsy, the ultrasound probe and patient movements cause the prostate to deform and change shape.
- The prostate is an organ that changes over time, often getting larger, therefore a delay between the MR scan and the biopsy can make overlay inaccurate
The original fusion systems merely overlaid one image with the over, but because of the issues described, the resulting fused image was not necessarily that accurate and required adjustment by the physician based on experience.
Elastic fusion
The latest software systems use common markers between the ultrasound and MR images to superimpose the MR image and automatically adjust the image so it better adjusts to the contours of the ultrasound image at that point in time.
As a result, elastic fusion, enables a more accurate display of the suspect areas previously identified on the MR scan. Further, it means far fewer biopsy samples are required making the procedure far less invasive.
Developers of fusion systems worth mentioning are Focal Healthcare Fusion BX, Koelis and Biopsee and BK Fusion.
However, fusion biopsy software is expensive and the process takes time. Therefore, its use is limited to a few centres.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media


