Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Screening for prostate cancer using biparametric (bp) MRI

Overview by Dr Aarti Shah
Consultant Radiologist
Basingstoke and North Hampshire Hospital
Hampshire Hospitals NHS Foundation Trust

and by Mr Simon Bott
Consultant Urological Surgeon
Frimley Health NHS Foundation Trust
MRI screening for prostate cancer – PI-RADS and MRI Parameters
A scoring system called PI-RADS (1) was introduced to standardize MRI evaluation to give a likelihood for prostate cancer being present. This system also gives recommendations for how optimal MRI for diagnosing prostate cancer should be performed.
Multiparametric MRI (mpMRI), which PI-RADS recommends as the standard of care for patients suspected of having prostate cancer, incorporates both anatomic and functional imaging – how the prostate looks and how much water or blood flow there is in parts of the prostate.
Anatomical imaging includes T1 and T2 weighted images whilst functional imaging, refers to diffusion weighted imaging (DWI) for water and dynamic contrast enhanced imaging (DCE) for blood flow. See examples below.
Each sequence will take a different amount of time and more sequences make for longer overall scanning times.
What is the difference between a bpMRI and mpMRI?
A biparametric scan ( bpMRI) includes T2 weighted images and DWI only whilst a typical mpmRI will include T2 weighted images, DWI as well as DCE. DCE also requires a separate injection of contrast medium.
A bpMRI is much quicker to obtain – 15/20 minutes as opposed to up to 45minutes with mpMRI. The shorter scans are cheaper and easier to perform and could therefore be more readily available in a variety of healthcare settings. This has significant implications at a population level.
Can we replace bpMRI with mpMRI?
Currently we use PSA to identify men who might need an MRI. MRI might one day become a method for screening patients for possible prostate cancer. Studies are ongoing to see if we can avoid the PSA and proceed directly to MRI scans or whether doing a PSA test can safely and more cost effectively avoid doing an MRI in most cases.
If an MRI is going to be undertaken does it need to be a full mpMRI or can we get similar results using a bpMR1? Several trials have sought to address this question.
Exciting new results from the PRIME trial presented by Dr Clare Allen in April 2024 show that in a multi-centre, international trial, if image quality is good, then the diagnostic performance of bpMRI and mpMRI is comparable. This is in the setting of men referred with a suspicion on prostate cancer. Other studies such as PACIFIC are also under way looking at this important area.
Separate studies have looked at screening populations which are very different to patient already referred for testing based on a raised PSA.
The first such study was the Prostagram undertaken at Imperial College led by Professor Hashim Ahmed. The results from a sample size of 490 men suggested that indeed bpMRI would be suitable. However it was determined that a much larger study was required to confirm these initial findings which should also take into consideration the potential importance of bio-markers. This has resulted in the landmark £42m TRANSFORM trial which will start this autumn and run for 10 years or so.
Conclusion
The evidence for bpMRI in the diagnosis of cancer seems strong currently. The use of bpMRI for screening at population level is less clear cut but will be answered in due course.
What remains very clear is that MRI when performed well and reported well is integral in the pathway of care for prostate cancer.

T2 weighted imaging : this is the workhorse of MRI and best for anatomical detail. Lesions will appear of low signal intensity.
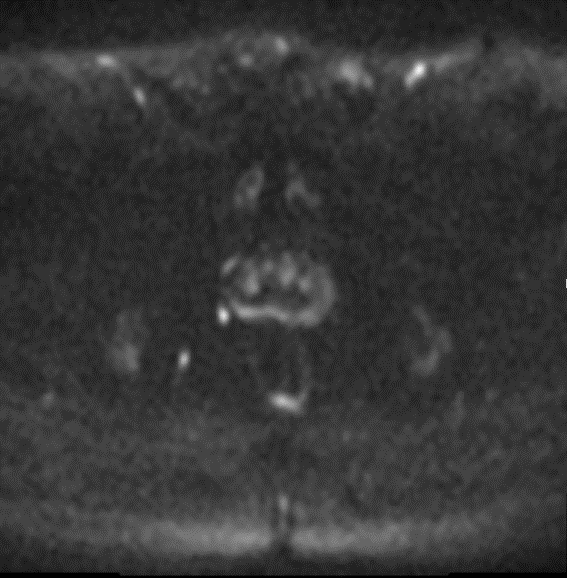

Diffusion Weighted Imaging (DWI) and Apparent Diffusion Coefficient (ADC) images are viewed together. Areas of high signal on the DWI images and low signal on the ADC images indicate ‘restricted diffusion’ – an indicator of a pathological process of cell death such as infarction, cancer, or abscess formation

Abnormal tissue, such as inflamed or cancerous tissue, is often more vascular than surrounding tissue and so ‘enhances’, appearing brighter on images after a contrast injection is administered.
References:
- Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ, Tempany CM, Choyke PL, Cornud F, Margolis DJ, Thoeny HC, Verma S, Barentsz J, Weinreb JC. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019 Sep;76(3):340-351. doi: 10.1016/j.eururo.2019.02.033. Epub 2019 Mar 18. PMID: 30898406.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

