Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Prostate cancer treatment – high and low dose brachytherapy

Overview by Professor Stephen Langley
Professional Director of Cancer Services,
Royal Surrey County Hospital
Co-Chairman Surrey & Sussex Cancer Alliance for Urology

Mr Rick Popert
Consultant Urological Surgeon
Guy’s and St Thomas’ NHS Foundation Trust
Prostate Cancer Treatment – Low Dose Rate Brachytherapy
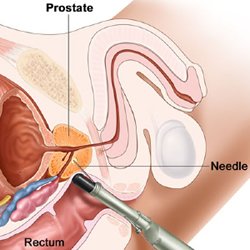
Brachytherapy is a bespoke form of radiotherapy in which delivery of radiation is targeted directly into the prostate gland by implanting small radioactive seeds under ultrasound guidance. Needles are inserted through the skin of the perineum. These needles are used to deliver the titanium seeds within which is the radioactive material, usually radioactive Iodine125. The individual seed positions can be planned very accurately with computer software to maximise the dose to the prostate whilst minimising the dose to the urethra or the rectal wall. The computer software systems can be used to optimise the dose to the most affected part of the prostate, as a “Focused” Brachytherapy implant.
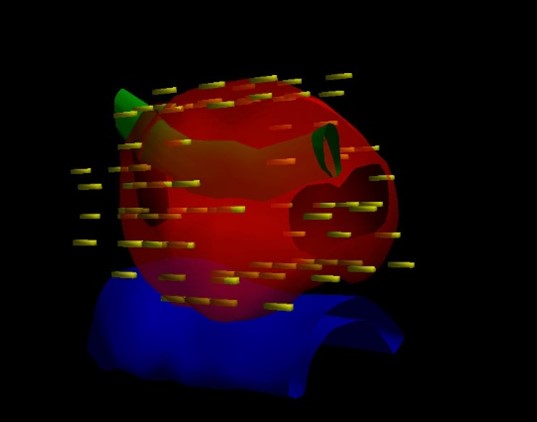
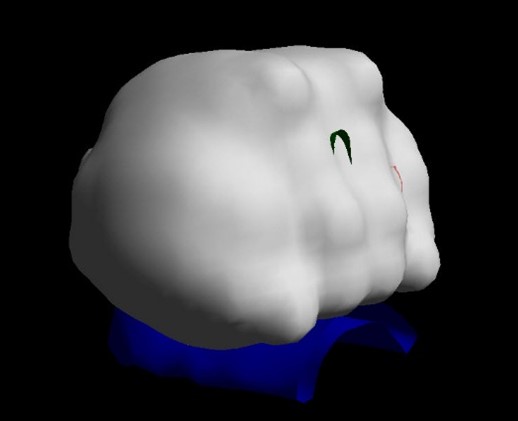
Brachytherapy planning computer images showing the outline of the prostate in red, the water pipe (urethra) passing through the prostate in green and the front of the rectal wall in blue. The simulated position of the seeds are shown in yellow and the resulting ‘cloud’ of radiation covering the prostate but sparing the rectal wall shown in grey. These images are created from the ultrasound images of the prostate obtained during the procedure enabling the position of the seeds to be optimised before implantation.
Brachytherapy is carried out as a day case procedure under a light general anaesthetic.
The procedure is usually carried out by a Urologist or a Uro-Radiologist and a Radiation Oncologist supported by a medical physicist. Brachytherapy treatments started in the late 80s and the outcomes reported at 10 – 15 years are equivalent to the best obtained by external beam radiotherapy or radical prostatectomy. With the advent of specialised MRI scanning and better targeted prostate biopsies Brachytherapy has become a highly refined and targeted prostate cancer treatment with little risk of incontinence and good preservation of erectile function.
Brachytherapy may be used as a primary therapy (monotherapy) or in combination with external beam radiation (EBRT) and or hormonal therapy, dependant on disease risk.
Patient Selection:
The ideal patient for brachytherapy should have no significant urinary symptoms (IPSS < 10), a normal urinary flow rate and a prostate volume < 60 cc, as measured by ultrasound assessment. Brachytherapy is not suitable for patients with large prostates (> 1000cc) because the pubic arch which sits in front of the prostate may obstruct the access of brachytherapy needles to the prostate gland. For patients with prostate glands between 60-100cc a short course of hormone therapy can be used to shrink the gland down to a size that is treatable.
A previous transurethral resection of the prostate is not a contraindication, but it will be necessary to document a urinary flow rate and carry out a cystoscopy to assess the prostate cavity.
Some patients who have urinary symptoms (IPSS 10 -20) related to benign prostate enlargement may benefit from a transurethral resection of prostate tissue to make them more suitable for brachytherapy. The brachytherapy implant is deferred for ~3 months and so these patients should have low to intermediate risk disease. Alternatively, those with higher risk disease will already have started their treatment which begins with hormone therapy. The 3 month period whilst the hormone therapy is given before the brachytherapy is an ideal time for patients to undergo a TURP and improve the urinary symptoms.
Low to Intermediate Risk Disease Gleason 3+3 or 3+4, ISUP Group 1 – 2.
Patients considered suitable for LDR brachytherapy as a mono treatment (single visit day-case procedure) normally have a PSA <15 ug/l, a Gleason score of 6 or 7 (ISUP Grade 1 – 2), with organ confined prostate cancer, stage of T1-T2b but multifocal disease such that they are not suitable for focal therapy but can still benefit from this less invasive treatment option.
Focal Gleason 4+3 (ISUP Grade3) may be suitable for a “Focused” brachytherapy implant in which the radiation dose is boosted to a very high level to maximise the dose to the involved quadrant whilst maintaining an overall standard treatment dose to the whole gland and avoiding the need for external beam radiotherapy. Such patients are usually treated with a short course of hormone therapy for 3 months before and after their brachytherapy.
Intermediate to High Risk Disease (Gleason score 4+3 or 4+5, ISUP Grade 3 – 4
Patients with higher risk cancer may be suitable for brachytherapy but in combination with hormone therapy and external beam radiotherapy as part of a multi modality treatment, For those men with higher grade disease and a high volume of disease, including up to T3a disease and a PSA is over 20, the hormone therapy may be continued after treatment for 2 years to maximise the chance of a successful outcome.
Men with the cancer extending into the seminal vesicles, (ie Stage T3B) are often best suited to be treated by High Dose Rate (HDR) brachytherapy, again in combination with both hormone therapy and external beam radiotherapy. This is because it is difficult to effectively treat the seminal vesicles with the radioactive seeds but this is not a problem for the HDR Technique
Low Dose Rate Brachytherapy (LDR)
The seeds used for LDR brachytherapy give off a low dose of radiation over 6 months, remaining in the prostate gland permanently, but inactive. This does no harm.
Brachytherapy in combination with a rectal spacer (SpaceOAR)
Brachytherapy can be combined with the insertion of a rectal spacer, such as SpaceOAR or. This is placed at the end of the brachytherapy procedure and involves the insertion of an access needle in to the fat filled space between the prostate and rectum. The two components of the SpaceOAR solution are injected together and immediately coalesce to form a gel matrix which separate the prostate from the rectum. This reduces the overall radiation dose effect to the rectal wall.
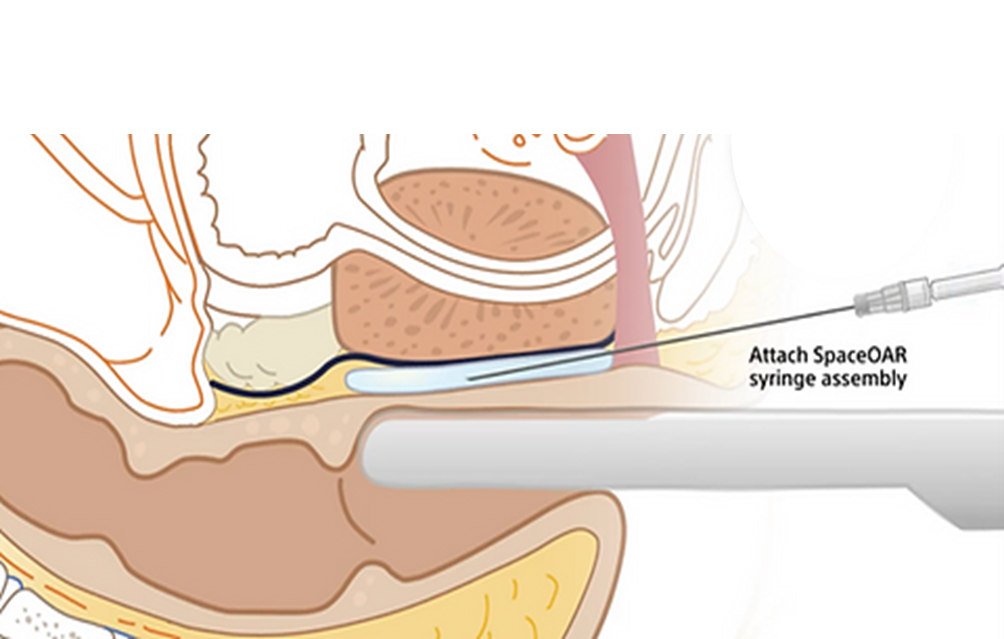
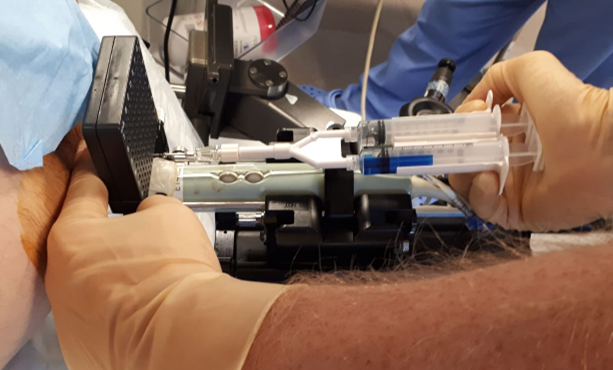
Photo and diagram showing a spacer gel being inserted transperineally throught the brachytherapy template at the end of the implant The gel separates the prostate from the rectum by ~10mm which significantly reduce the radiation dose received from the rectal wall.
High Dose Rate Brachytherapy (HDR)
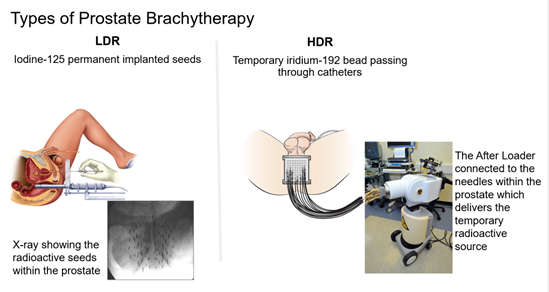
In HDR brachytherapy fine hollow needles are inserted through a template (the same as used for template guided biopsy), and the perineal skin, and into the prostate gland. Typically 16 needles are used which are then attached via tubes (catheters) to an After Loading device that houses the radiocated source a bead of iridium192
The radioactive bead isthen inserted and withdrawn from each needle in sequence . A computer controls the length of time the source stays in each needle so allowing the radioactive dose delivered to the prostate to be accurately tailored to the shape of the gland.
After treatment the needles are removed, leaving no radioactive material in the prostate gland. Although the treatments can be delivered in one day patients are often in hospital for two days and on occasions the procedure is performed more than once. HDR brachytherapy is normally given to boost the radiation dose to the prostate as part of a multi-modal treatment involving both hormone therapy and external beam radiotherapy
Advantages of brachytherapy treatment
- Cure rates in low risk patients are equivalent to surgery or External Beam Radiation Therapy (EBRT)
- For intermediate and high risk patients, when combined withhormone therapy and or EBRT cure rates are better than for surgery or EBRT alone.
- The procedure is carried out as a day case and there is no need for a catheter
- No incisions or stitches are required
- Minimal, if any, post operative pain
- Incontinence rates are less than 1%
- Over 80% of men who are potent with good erectile funtion before treatment will maintain their erection
- Normal tissues nearby may receive a smaller dose of radiation compared with treatment with external beam radiotherapy, and therefore are less likely to be damaged.
- Recovery is quick, which means you can return to your normal activities within a few days.
Disadvantages of brachytherapy treatment
- The most common side effect is temporary urinary irritation including frequency and urgency. These symptoms will last from a few weeks to a few months and are helped by medications, such as alpha blockers.
- It may be some time before you will know whether the treatment has been successful. The PSA is checked every 6 months and it can fluctuate in the first 18 months (PSA bounce). A PSA bounce occurs more commonly in younger men and is often a sign that the treatment is having an effect on the prostate cells, generally by 3 years the PSA is at a very low level.
- With LDR brachytherapy the radioactive seeds stay inside the body permanently and emit radiation for 6 months but after they are inert and cause no problems.
- With LDR brachytherapy it is possible that individual seeds may move out of the prostate to elsewhere in the body or you may pass them in the urine, but because the dose emitted by an individual seed is so low this causes no harm and does not affect the overall treatment. Some techniques such a 4D brachytherapy which uses seeds linked together in an absorbable strand of material around the outside of the glad can avoid this risk of seed migration
- HDR brachytherapy may require more than one radiation treatment so you may need to stay in bed for at least six hours between treatments with the tubes in your prostate. Some men find this uncomfortable and you may need to stay in hospital overnight for HDR treatments.
The Difference between High Dose Rate (HDR) Brachytherapy and Low Dose
Rate (LDR) Brachytherapy.
Brachytherapy is a technique to deliver radiation into the prostate gland to treat prostate cancer. The term brachy is derived from Greek, meaning short, i.e. there is a short distance for the radiation to travel to reach the cancerous gland, unlike conventional radiotherapy where the radiation is shown from a large machine, linear accelerator, through the body to reach the prostate. The advantage of placing the radiation directly into the gland, is that higher more effective doses can be delivered without irradiating surrounding structures. There are two forms of prostate brachytherapy, Low Dose Rate and High Dose Rate. Low dose rate does not mean a low dose is given, but refers to the speed of the delivery of the radiation dose. In high dose rate brachytherapy the dose is given quickly over ~30 minutes via needles temporarily inserted into the prostate, while the patient is under anaesthetic, a so called temporary implant. In low does rate brachytherapy the dose is delivered over 3-4months via tiny radioactive seeds which are permanently implanted into the prostate under a short anaesthetic.
In the UK, the seeds use iodine 125 as their radioactive source. The seeds are tiny canisters of titanium, which is inert in the body, and sealed inside these canisters is the radioactive iodine. Typically 60-100 seeds may be used to treat a patient, the actual number depends on the size and shape of their gland. When all the radiation is emitted the inert titanium seeds remain permanently within the prostate. The procedure often only takes 30-45mins and for the patient is a similar experience to having a prostate biopsy, except they are usually under a general anaesthetic.
In high dose rate brachytherapy the radioactive source is Iridium192. The source passes from a holding device called an After Loader into each needle in sequence. There are typically 16 hollow needles inserted into the prostate and a computer moves the source in and out of each needle in turn. The whole procedure usually takes 2-3 hours and may be performed twice on different occasions. The patient is often kept in overnight with a urinary catheter in place before being discharged, catheter free in the morning
Both HDR and LDR brachytherapy are very effective treatments for prostate cancer. The data is most mature and established for LDR Brachytherapy with outcomes data reaching 20 years now published. They tend to be used in different ways. LDR Brachytherapy may be used as a stand alone treatment for men with low and favourable intermediate risk prostate cancer. For those men with higher intermediate risk disease it is sometimes combined with a short course of hormone treatment as well, to improve its efficacy.
For men with higher risk prostate cancer it may be given in a ‘trimodal’ approach in combination with both hormone therapy and a short course of external beam radiotherapy. There is good research data to show that such combined treatment is more effective at treating the prostate cancer than if just external beam radiotherapy and hormone therapy are used in combination.
HDR Brachytherapy alone as a single treatment has been shown not to be as effective as other therapies. The technique tends to be used in combination with hormone therapy and external beam radiotherapy as a way of boosting the radiation dose to the prostate gland. It is especially well suited to treat patients where the prostate cancer has spread into the seminal vesicles (i.e. stage T3b) as it is difficult to boost this area with radioactive seeds.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

