Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Prostate cancer diagnosis – the Old Pathway: TRUS and its limitations

UCLH Westmoreland Street
University College Hospital London, NHS Trust
Prostate Cancer Diagnosis – the Old Pathway
Problems with trans rectal ultrasound biopsy
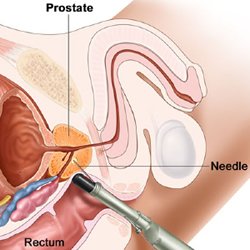
Following a Urology referral, the standard pathway was to offer prostate biopsy to men who are at risk of prostate cancer, due to either a raised prostate specific antigen (PSA) or an abnormal feeling prostate on an examination done by a doctor – Trans Rectal UltraSound guided prostate biopsy (TRUS). It continues to be the pathway used in many urology centres although it has now been superseded by a far superior approach. A TRUS is done by inserting an ultrasound probe into the rectum and taking up to 12 samples of tissue from all regions of the prostate. (See illustration) It has a small risk of bleeding or infection, is usually uncomfortable, and sometimes painful.
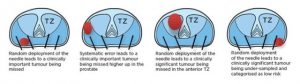
The samples are taken from standard places in the prostate to try and cover as much of it as possible – often called ‘random’ as the clinician doing the biopsy cannot see in which precise area they are taking each biopsy core. This makes the diagnosis of prostate cancer using this method rather unusual, as it is virtually the only cancer that is looked for by sampling the entire organ without seeing or feeling the abnormality. We could make an analogy with breast cancer: no one would consider random biopsies of the breast without knowing where a suspicious lump was. The prostate is of course much smaller, and many cancers are picked up by random sampling, but some, especially at the front of the prostate, are missed entirely.
If a cancer is found, the standard pathway usually included an MRI scan to see whether the cancer has gone outside the prostate or to the lymph nodes – to ‘stage’ the disease. A TRUS biopsy does not provide enough information to determine whether a patient is suitable for Focal Treatment.
Problems arising from transrectal biopsy
- Transrectal biopsies can over-diagnose clinically insignificant prostate cancer.
A man who undergoes transrectal biopsy has a 1-in-4 chance of being diagnosed with prostate cancer – most of these cancers tend to be the indolent type that men die with and not from.
- Transrectal biopsies can miss clinically significant cancers.Due to their random nature, they have an estimated false negative rate of 1-in-3. Men who test negative for prostate cancer are either discharged to the community for yearly PSA testing or the same unreliable and harmful test can sometimes be repeated several times over a number of years in one man.
- Transrectal biopsies can be unrepresentative of the true burden of cancer.1-in-3 men deemed low risk on transrectal biopsies can have higher volume or grade cancer, or both when a more accurate biopsy test is applied. The attribution errors of transrectal biopsy result in inappropriate treatment allocation—men with high-risk disease might be recommended conservative management in contrast to radical therapy, and men with low-risk disease are recommended radical therapy ‘just in case’.
- Transrectal biopsy can cause harm. Three-quarters report at least one minor complication after prostate biopsy. see the table below.
Risks and complications from transrectal biopsy
INFECTION
Bacteriuria: 20%-50%
Bacteremia: 20%-70%
Urinary tract infection: 1-8%
Life-threatening sepsis: 1-4%
BLEEDING
Haematuria: 50%
Haematospermia: 30%
Rectal bleeding: most
URINARY OBSTRUCTION
Acute urinary retention: 1%-2%
Voiding symptoms: 10%
VASOVAGAL REACTION 8%
Where to Start

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

