Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Techniques to reduce the side effects of robotic prostatectomy

Mr Prasanna Sooriakumaran (PS)
Consultant Urological Surgeon
University College London Hospitals NHS Trust (UCLH)
Innovations in prostate cancer surgery – to cure whilst minimising side-effects of robotic prostatectomy
Prostate cancer is the commonest cancer affecting Western men, and is twice as common in Black men as White men and in those with a father or brother who had it. The average White man has a 1 in 8 risk of getting significant prostate cancer in his lifetime; this doubles to 1 in 4 if his father or brother had it. The average Black man starts with a 1 in 4 lifetime risk which doubles to 1 in 2 if his father or brother had it. This means that prostate cancer is now very common, and becoming even more common with time, as men live longer and stop dying from other causes as much. It is a common misconception that prostate cancer is no big deal, and you can live with it without having any treatment. This may indeed be true for the ‘insignificant’ prostate cancers, what I like to call the ‘pussy-cats’. But many prostate cancers are much more aggressive, like ‘Bengal tigers’ if you’ll indulge my analogy, and thus need treatment.

Some prostate cancers are insignificant or “pussycats” whereas many need treatment (the “tigers”)
So, if you are patient reading this, the first thing you need to ask your urologist once you’ve been given the unfortunate diagnosis of prostate cancer, is what type it is- a pussy-cat or Bengal tiger or something in between? Now, the ‘pussy-cats’ can be managed with active surveillance, but the ‘big cats’ need treatment. Focal therapy may be appropriate for a minority of these cancers, but it is important to know that it can result in worse outcomes should it fail (needing another focal therapy or other treatment occurs in 1 in 4 men at 5 years of follow-up so it can have a high failure rate). It is also important to know that focal therapy is considered experimental or investigational by the 2 most prestigious international urology societies, the American Urologic Association (AUA) and the European Association of Urology (EAU). So, while many UK colleagues are ardent supporters of focal therapy, independent sources with no ‘skin in the game’ are rather more cautious in recommending it.
So what are the tried tested treatments for significant prostate cancer that the AUA and EAU do recommend? Well these fall in to 2 broad groups: surgery and radiotherapy. The latter is dealt with in another section so I won’t expand on it, but the former is considered the ‘gold standard’ treatment for most young, fit men with significant prostate cancer. While surgery sounds scary to many men, I want to reassure you that there have been huge advances and innovations in surgical treatments that have really reduced the side-effects without compromising effectiveness. The advent of robotic surgery is one of these advances, and I was privileged to train under an American urologist who was in the team that pioneered the very first of these robotic prostate cancer operations, the so-called ‘robotic-assisted radical prostatectomy’ or RALP. I also trained under a European pioneer who popularised RALP across Europe, and these two trainers have collectively done over 10,000 RALPs! This means I have benefited from their huge experience, which I have transferred to my own surgical techniques. So, the next question is what are those robotic techniques that have improved outcomes for men?
The use of Retzius-sparing RALP is probably the most important innovation of all. This technique allows virtually no disruption to the supports of the bladder (as the surgery doesn’t enter the ‘Retzius space’ where the bladder sits) during the surgery, which leads to swifter recovery of urine control (‘continence’) after the operation. Studies from many international experts have demonstrated this benefit over standard RALP conclusively. Santis, the highest volume private prostate cancer centre in the UK, performs more of these Retzius-sparing RALPs than any other private centre in the UK, and our results show these benefits for UK patients. The Santis data on this will be presented at international urology conferences across America, Europe, Asia, the Middle East, and the UK. In fact, I am about to start a UK-wide study examining the benefits of the Retzius-sparing approach for patients undergoing RALP. I will lead this study and we will include patients from as many UK surgeons doing this technique as possible, rather than just a few Santis surgeons. The main downside of the Retzius-sparing technique is that it is difficult to do technically, and thus many surgeons are not comfortable doing it. As is human nature, they thus tend to underplay its benefits or rationalise why it’s not a good technique. However, it is a good technique. Though it shouldn’t be used for all men undergoing RALP as certain prostate anatomy and cancer anatomy makes it less effective; in these cases, I will still perform the standard RALP. So, like with many innovations, it needs to be carefully selected for certain patients. It might therefore be worth checking whether your surgeon offers this technique and if not, go and see someone who does. Even if it ends up not being appropriate for you, that decision is best made by a surgeon skilled at it rather than one who never does it and thus will never recommend it.
Other innovations in RALP surgery that have resulted in men’s erections returning stronger and quicker than they did with conventional surgery, are grades of nerve-sparing and Neurosafe. Grades of nerve-sparing is a concept I helped develop with my American mentor (yes, the one who’s done zillions of cases), and allows the surgeon to accurately spare nerves in a ‘graded’ manner. What I mean by this is that nerve-sparing is not an ‘all or nothing’ phenomenon, but rather the nerves lie along the side of the prostate in different layers, rather like the peel of an onion. Each different layer of the ‘onion’ has nerves within it and thus a skilled surgeon in the ‘grades’ technique can spare all the layers, none of the layers, or some of the layers, and this will result in differing amounts of nerve sparing, and thus better erections for patients after surgery. An Oxford study I am senior author on that is ‘hot off the press’ has shown the benefits of this grades of nerve-sparing technique on the recovery of erections without any compromise on cancer control.
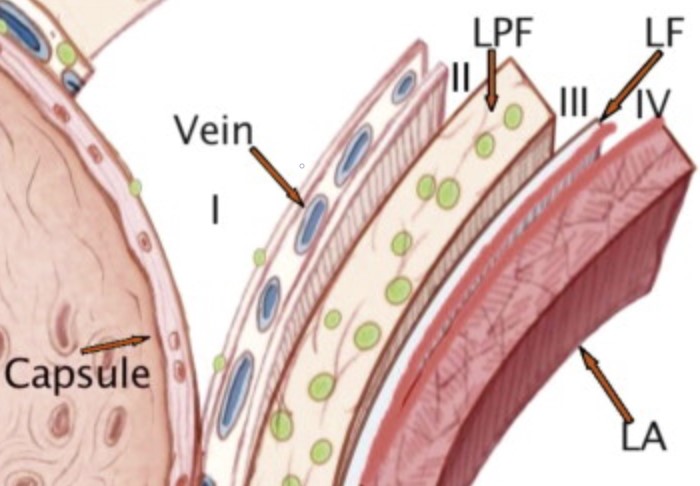
Nerves on the surface of the prostate lie within different layers and thus “nerve-sparing” can be graded instead of an “all-or-nothing” approach adopted by some surgeons
Another technique offered by all Santis surgeons, and pioneered by my German collaborators whom I work very closely with on a number of prostate cancer projects, is Neurosafe. This is a technique whereby all the nerves are spared at the time of surgery and then the edge of the prostate is snap-frozen and examined by a pathologist during the operation. If there is no cancer at the edges, then the nerves can be left spared and the operation completed. However, if there is cancer on the edges, then the nerves are then removed before the operation is completed. The advantage of this approach is it allows full nerve sparing; the disadvantage though is that the snap-frozen result is not 100% accurate so mistakes can be made, and if the nerves then need to be removed they are ALL removed. The ‘grades’ approach on the other hand allows far more ‘personalisation’ in that some nerves can be spared, rather than an ‘all or nothing’ approach based on the Neurosafe ‘frozen’ results which might be inaccurate. So, again, like for the Retzius sparing versus standard RALP issue, it is important for surgeons in my opinion to be skilled in both ‘grades of nerve-sparing’ and Neurosafe operations, and to personalise the technique based on the cancer anatomy and the wishes of the patient.
So, with innovations that further improve continence and erection outcomes after RALP, this surgery in skilled, experienced hands is likely to remain the “gold-standard” for the young, fit man with significant prostate cancer.
But what are the limits of robotic surgery? There are 2 categories of prostate cancer where surgery wasn’t commonly used and is now being used more and more. The first is for patients who have failed other treatments; this surgery is called ‘salvage’ because the surgeon is trying to salvage the situation. Salvage RALP after radiotherapy has more complications and side-effects than RALP done as the initial treatment because of the scarring (‘fibrosis’) caused by radiotherapy. However, there are skilled and experienced RALP surgeons (e.g. those working at University College London Hospital (UCLH) or the Santis Clinic) who have excellent outcomes for patients who undergo this challenging surgery in their hands. Another challenging patient for RALP surgery is the man with metastatic disease. Recent data from the largest interventional prostate cancer study in the world, STAMPEDE, which I am one of the urologists on has shown that local treatment to the prostate can improve survival in some men with advanced (so-called ‘metastatic’) cancer that has already spread to lymph nodes and bones. I have led an internationally-acclaimed, internationally-funded, award-winning study called TROMBONE that showed benefits in quality of life outcomes for men who underwent robotic prostate cancer surgery (RALP) for advanced prostate cancer. This study has made the national and international press on multiple occasions, and continues to do so. It means I have one of the world’s largest experience of operating on men with advanced prostate cancer, and UCLH was the highest volume centre involved in this study.
So, to sum up, we have developed innovations in robotic surgery that improve continence and erection outcomes after prostate cancer surgery. We have expanded the indications for robotic surgery to include failures of other treatments and for some men with advanced, or metastatic, prostate cancer. But it is important to remember that not all surgeons should do all these kinds of complex cases. Only as a surgeon gets better and more experienced at a skill, should they do complex cases like this. That makes sense, right? When I first learnt to play golf I only played 9-hole, par 27 courses. Now I can play on standard 18-hole Par 72 courses. One day, I hopefully will be good enough to play on championship courses. The same is true for robotic surgery; the most complex cases like the salvage and metastatic cases should be done by the most skilled and experienced surgeons in the most skilled and experienced centres, such as like UCLH and Santis to minimise side effects of robotic prostatectomy.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

