Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Intensity-Modulated Radiation Therapy (IMRT)

Overview by Overview by Dr Philip Camilleri
Consultant Clinical Oncologist
Oxford University Hospitals NHS Trust
and
Clinical Director – Urological cancers and MR Linac
Genesiscare UK
IMRT for prostate cancer
What is intensity modulated radiotherapy (IMRT)?
IMRT is the ability to shape the high dose beam of a radiation machine or linear accelerator (linac) to the shape of the target or tumour being treated. This requires specific software and hardware installed onto the linac to allow delivery of highly accurate, sculpted high dose areas. Results from long-term follow-up studies of men with prostate cancer who were treated with IMRT are impressive when compared to standard external beam radiotherapy (EBRT)
Studies of diverse groups of patients including those who commenced treatment with high PSA and Gleason scores, demonstrate that up to 10 years later, the overwhelming majority have neither recurrence of the original cancer nor have they developed new cancers – which might be expected given the high doses of radiation used in IMRT. Further, because the radiation is delivered so accurately, thereby minimising the radiation exposure for normal tissue, incidence of damage to the bladder which can cause incontinence, or bleeding due to damage to the rectum, is low.
For this reason, IMRT is regarded as the current NHS standard for radiation treatment of prostate cancer and is available across the board in all NHS Trusts.
How does IMRT work?
Nearly all radiation technologies use linacs to produce high energy X-ray beams which are targeted on the tumour. The two main manufacturers are Elekta and Varian although more recently newer, more technologically complicated linear accelerators have been developed to further enhance the accuracy of the treatment delivered. These include the CyberKnife by Accuray and MR guided linear accelerators such as the MRIdian by ViewRay and the Elekta Unity. The latter machines are dealt with on our page regarding stereotactic radiotherapy (SBRT)
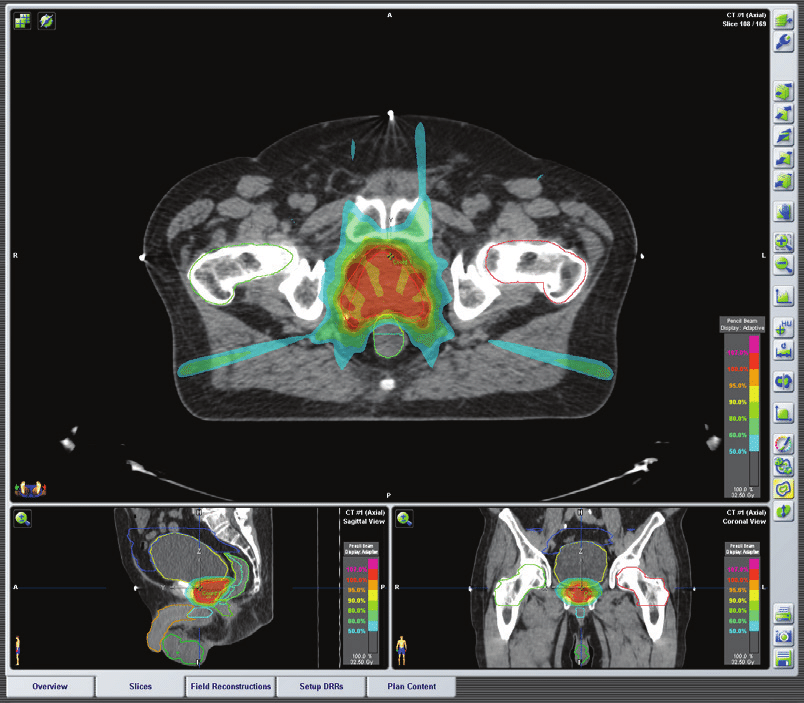
IMRT systems are high precision in terms of targeting the radiation onto the tumour or specific areas within the tumour. This is achieved by computer-controlled delivery systems which allow the radiation dose to conform very precisely to the shape of the tumour by modulating or changing the intensity of the radiation beam. This allows the radiation to be targeted on the cancer whilst reducing the damage to normal tissue and structures in the surrounding area.
Treatment is planned using MRI and CT images to determine the size and shape of the tumour. This information is then used to compute dose calculations and dose intensity patterns that will best attack the tumour. The beams are delivered from several directions at different intensities, customizing the treatment for an individual patient. IMRT is often combined with androgen deprivation therapy also commonly called hormone therapy. In addition, IMRT can sometimes be combined with a boost of radiation delivered directly into the prostate using a technique called brachytherapy. (See page on Brachytherapy). Often the IMRT portion is given over a period of three or four weeks and can be either preceded or followed by a brachytherapy boost using either permanent low dose rate (LDR) seed implants or a temporary high dose rate (HDR) implant over a 30 minute session. If you have higher grade disease and volume of disease this combination treatment will often be combined with a minimum of 24 – 36 months hormonal therapy.
Additional technologies
Potential toxicity to normal tissue is further reduced by injecting a synthetic hydrogel called SpaceOAR (manufactured Boston Scientific) as a spacer between the prostate and rectum. This moves the rectum away from the prostate by a small amount (usually 10-12mm) which is just enough for the rectum to be moved out of the high dose area of the radiation field.
The gel is inserted under local or general anaesthetic in a short outpatient procedure, via a single needle into the perineum. The gel is non-toxic and will stay in place without degradation for approximately 3 months. It then begins to be reabsorbed by the body over the next 3 months and within 6 months of being inserted it has usually been eliminated by the body through the urine. The gel does not cause any pain or discomfort while in place although patients do report a slight feeling of fullness in the rectum initially.
Evidence shows that it reduces long term side effects to the bowel by around 50% and also seems to help reduce urinary and erectile dysfunction side effects as well to some extent.
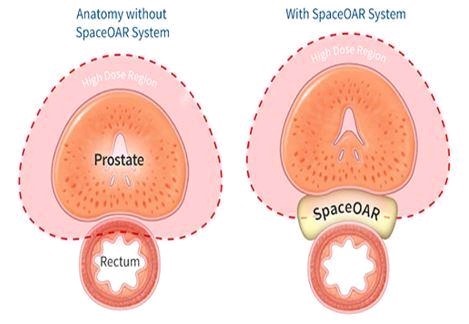
Image Guided Radiation Therapy (IGRT)
IGRT refers to the use of imaging, usually CT scans and X-rays and sometimes with MRI scans, to help precisely target the cancer with radiation therapy. With IGRT on a standard linac, CT scans or X-rays, or both, are taken every day before each radiation treatment to ensure that the cancer or region to be treated is exactly in the same place each day of treatment. IGRT is always used when IMRT is being used. The patient is ‘set-up’ meaning asked to lie on the treatment couch on their back in the same position every day. A quick X-ray or CT scan is taken using special equipment mounted on the treatment machine.
In order to help the accuracy of the image guidance, sometimes small markers made of a highly visible metal (eg gold) are inserted into the prostate under local anaesthetic a couple of weeks or so before the start of radiotherapy. The gold markers are inert and therefore do not interfere with the body in any way. They are not radioactive and will stay in place in the prostate without causing any concern for the rest of the patient’s life. Adjustments can be made prior to each treatment to make certain the prostate is adequately covered by the radiation beams and to check that surrounding normal tissue or organs are not receiving too much dose.
When radiation therapy is being given for prostate cancer, the prostate gland can move slightly inside the body depending on how full or empty the lower bowel (rectum) and bladder are. Using a CT scanner called a Cone Beam CT, built into the treatment machine, any movements of the prostate can be seen prior to each daily treatment. Alternatively, the position of the prostate can be seen from the position of the gold markers and the position adjusted quite quickly and accurately without needing a further Cone Beam CT (CBCT) scan.
How long does it take to be treated?
IMRT is usually given five days a week for between four to eight weeks.
The exact number of treatment sessions and radiation dose depends on the size and location of the prostate cancer and the health of the patient.
The reason for breaking the treatment up over several weeks is to minimise the damage to normal tissue by delivering relatively small doses each day. There is no treatment on two days out of every 7 day and this is usually over the weekend. The weekend break allows normal tissues to recover.
Side effects
Common side effects are as follows:
- A feeling of urgency when needing to urinate meaning having difficulty postponing passing water.
- Passing water more frequently during the day and night
- Poor flow and a burning sensation when passing water
- Looser, more frequent bowel movements.
- A feeling of urgently having to have a bowel movement and being unable to postpone.
- Bleeding visible on opening the bowels either on the stool or on the toilet paper.
- Irritation of haemorrhoids with a temporary worsening.
- Fatigue and tiredness are also common but improves after treatment.
- Erectile dysfunction.
Most men do not have problems with erections or intercourse during or right after IMRT. Over time, erections may become fewer due to long term impairment of the nerves near the prostate that facilitate erections. Commonly however erectile dysfunction occurs as a result of hormone therapy and can become permanent after radiotherapy.
Fertility
IMRT may result in the production of less or no seminal fluid. This is because the prostate’s function is to produce the fluid that sperm swim in and is the bulk of the fluid expelled at ejaculation. Because the prostate can no longer function after radiotherapy, the fluid diminishes until it disappears. If still able to achieve orgasm, this is commonly a little different and is called a dry orgasm. Radiotherapy can both damage sperm and reduce sperm count resulting in infertility. For this reason, if fertility is an issue, sperm is collected and frozen for future use prior to IMRT treatment. Having said this for most men who develop prostate cancer, this is rarely an issue.
If you have any comments or suggestions for improvement to this information please do not hesitate to contact us.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media

