Prostate matters is a not for profit organisation committed to providing free information about prostate issues from leading Clinical Authorities.
Prostate cancer diagnosis – the new pathway

UCLH Westmoreland Street
University College Hospital London NHS Trust
Prostate Cancer Diagnosis – the New Pathway
The ‘gold standard’ or the best way to diagnose prostate cancer is a 3T multiparametric MRI (mpMRI) and an MRI-targeted transperineal biopsy in those that need it, with additional samples taken from areas that look normal on MRI.
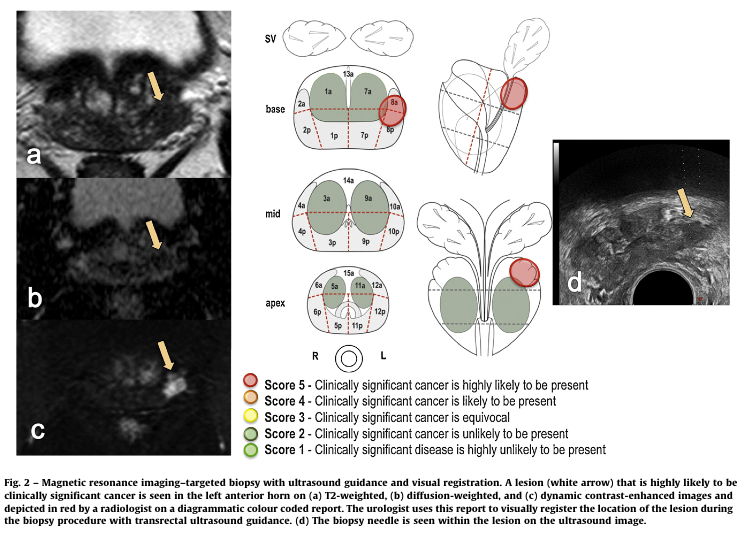
The MRI scan should be multi-parametric ie it should use a number of parameters, including anatomical imaging (T1 and T2 –weighted); diffusion weighted imaging (which assesses the movment of water, which we know is restricted in areas of cancer) and contrast enhanced imaging (many prostate cancers take up contrast quickly and release it quickly, because of their good blood supply).
The MRI will be assigned a score. Any areas scoring 4 or 5 should be biopsied, as a cancer is likely (but not definite) in these areas. When an MRI has a score of 1 or 2, it is possible to avoid a biopsy, and monitor the PSA. When the MRI score is 3 (equivocal) then the decision to have a biopsy or not will also depend on other factors, such as the PSA density.
When a decision to do a biopsy has been made, then the way that the biopsy is done should be considered. The traditional biopsy (done without an MRI first) uses an ultrasound probe in the back passage (transrectal ultrasound) to see the prostate. Needles are passed along the probe , through the rectal wall, to take small samples of tissue from the prostate. As the needles go through an area which is difficult to clean, there is a risk of infection – this can be up to 2-4% of men needing treatment in hospital. If an MRI has not been done, then a systematic biopsy will be carried out – taking samples according to a standard plan – often 6 cores from the right and 6 from the left.
If an MRI has been done then a transrectal approach can be used to target the lesion seen on MRI, and to take systematic samples as well. The MRI information can be used at the time of the biopsy in one of 3 ways:
- Visual registration – the biopsy operator looks at the MRI scan, and the radiologists report, and used landmarks visible on ultrasound to locate the area of interest.
- Software assisted registration – computer software is used to show the MRI lesion on the ultrasound image – this is sometimes called image fusion.
- Doing the biopsy in an MRI scanner. This will usually involve doing a diagnostic scan to assess the prostate, and then using a lower strength magnet where MRI-compatible needles can be used, to locate the lesion at the time of the biopsy.
None of the ways has been shown to be better than another, so that those who use software to target an MRI lesion have similar rates of cancer detection as those who are expert at biopsying using visual registration. We know that if both approaches are used in the same patient (and so more cores are taken) then the likelihood of finding a significant cancer is slightly higher than using one approach alone.
Biopsy approach – transrectal or transperineal
Biopsies can be taken either via the rectum (transrectal biopsy) or through the perineum, which is the skin between the back passage and the scrotum (transperineal). The transperineal method has a lower risk of infection (0.2% compared to 2-4%) than a transrectal approach.
Biopsy plan – targeted + systematic or systematic alone
Biopsies can be done in a targeted manner (ie taking multiple samples from an area of suspicion on MRI), or in a systematic manner. When systematic biopsies are done transrectally it is common to take 5 or 6 cores from each of the right and left side of the prostate.
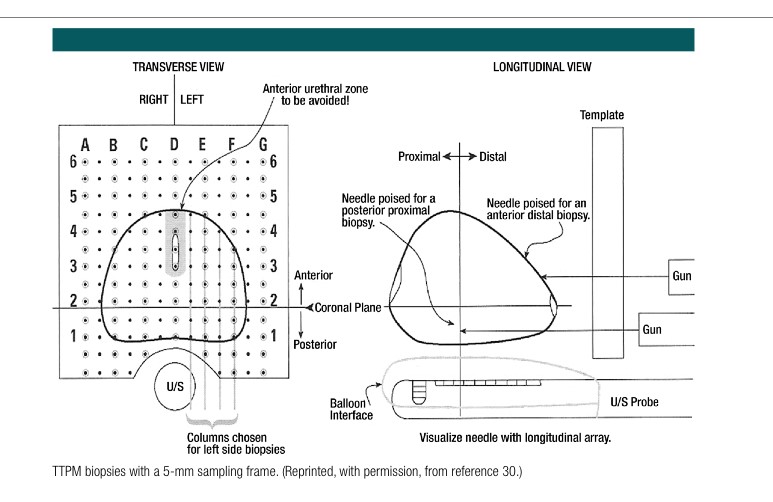
When systematic biopsies are done via a transperineal approach this is often done using a plastic square called a template. One way of doing a transperineal template guided biopsy is to take samples at every hole in a 5mm grid (a 5mm template mapping biopsy) – this is very rarely needed outside of a clinical trial. Another systematic transperineal approach is to take samples in 12 sectors, with one or two samples per sector. This would be suitable for men who cannot have an MRI eg due to a pacemaker.
When targeted biopsies are done, it is common to take some additional samples from the other side of the prostate, concentrating on the peripheral zone where cancers are more commonly seen.
For those hospitals that have a transperineal only approach, this can be done either under local anaesthetic (an injection in the skin and tissue around the prostate) or with additional sedation, similar to a light general anesthetic. It is common to allow patients to choose between local anaesthetic or sedation.
Trans-Perineal Biopsy. In the past couple of years this has replaced the TRUS Biopsy.
The MRI scan
Non-invasive mpMRI scans and reports provide a picture of potential cancer lesions. For about a third of patients the mpMRI shows the chance of significant disease is so low that no further investigation is required.
Whilst 3T MRI provides the best quality image, only a few centres have these machines. A 1.5T MRI is acceptable as long as it conforms to the agreed standards, such as those set out in a recent Consensus Paper standard, which covers the protocols and reporting of the mpMRI scan.
Later sections provide more information on the mpMRI and Trans-Perineal biopsy as well as hospitals, clinics, and surgeons that use this standard.
The New Pathway
There have been a number of studies which have helped to change the way that prostate biopsies are done. Two of these were carried out by teams in the UK, based at University College London. The PROMIS study compared MRI with both the standard transrectal biopsy and a 5mm template mapping biopsy. It showed that twice as many cancers were seen on MRI than using a standard biopsy, when both were compared to the very detailed mapping biopsy. However, we know that men having a 5mm template mapping biopsy can have significant side effects from the biopsy alone.
The PRECISION study randomised men to either a standard biopsy or an MRI, and a targeted biopsy in men who had a suspicious area on MRI. Men who had an MRI scoring 1 or 2 did not have a biopsy. This showed that an MRI-targeted biopsy found more of the clinically significant cancers and fewer insignificant cancers than the standard approach, and that around 1 in 4 men could avoid a biopsy if they had an MRI that was low risk.
Challenges
The current NICE Guidelines – from 2014 – have been superseded. Each NHS Trust is doing the best it can, given the equipment they have locally, and the available expertise. This can mean that some NHS Trusts are not able to provide current best practice, in terms of the diagnostic pathway they offer

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
In memory of Riki
PROSTATE MATTERS
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk
Site design and technical development by Webtoys | Intelligent Digital Media